By Helena Oliviero – The Atlanta Journal-Constitution
J. Scott Trubey – The Atlanta Journal-Constitution
Ariel Hart – The Atlanta Journal-Constitution
Troy Warren for CNT #Health #COVID-19
Coronavirus infections have reached record levels in Georgia. Though omicron causes a more mild illness for many, especially the vaccinated, it’s so contagious, it’s overwhelming hospitals and pushing the health care system to the brink.
But this wave is also different. Here’s a look at what Georgia doctors have to say about what they’re seeing in their practices and hospitals and the latest wave of cases.
Q: What is the latest trend line of infections and when might Georgia peak?
A: The omicron wave has set new records across the nation and in Georgia for new infections, more than doubling any previous peak. There are signs the outbreak is slowing or perhaps on the decline in core Atlanta area counties, but it’s still raging in counties outside the metro area.
As high as the numbers are, Dr. Felipe Lobelo, an epidemiologist at Kaiser Permanente of Georgia, thinks the official counts are only detecting 10-20% of the actual cases because so many people are taking rapid tests at home and those results aren’t part of the official count.

The super contagious omicron coronavirus variant “will ultimately find just about everybody,” Dr. Anthony Fauci, the nation’s top infectious disease expert, said this week.

Many experts believe COVID-19 cases may soon drop dramatically as the omicron wave reaches its peak. Overall in Georgia, Lobelo expects cases might peak this week, but hospitalizations, which tend to lag behind cases, may not reach the highest number for another week or two, he said.
Q: How well are vaccines holding up against omicron?
A: Unlike the delta variant that hit Georgia in August, omicron seems to cause much higher numbers of breakthrough cases. Breakthrough infections — infections in people who are fully vaccinated and, in some cases, even boosted — have been on the rise for months as omicron has taken hold.
But the vaccines are still highly effective at preventing severe illness. Preliminary data about omicron suggest two doses of the Pfizer vaccines are around 70% effective at preventing severe disease. Boosters are shown to increase effectiveness against transmission and severe infection.
The vast majority of COVID-19 patients hospitalized are unvaccinated. At Northeast Georgia Health system, 82% of ICU COVID patients were unvaccinated, according to the most recent statistics published on the hospital’s website. At Children’s Healthcare of Atlanta, 88% of children hospitalized for COVID-19 are unvaccinated, according to recent statistics.

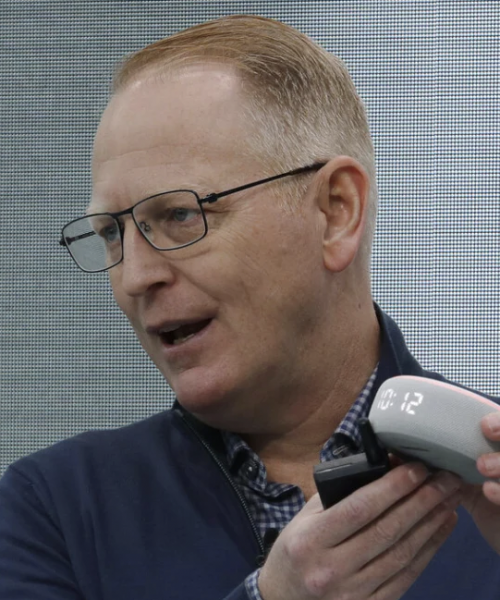
Q: Questions have been raised about COVID-19 patient numbers being artificially driven higher by patients who are hospitalized with something else but also test positive for COVID-19. Robert Jansen, chief medical officer, of Grady Health System discusses how rampant spread puts a stress on a hospital system.
A: “There are some of those,” Jansen said of incidental COVID-19 diagnoses. ”Certainly, some of the trauma patients and some (obstetrics) patients come in and just happen to be positive. I think what you are seeing though is people coming in with exacerbation of their underlying chronic diseases that are made worse by COVID.”
“So people who have underlying chronic lung disease or diabetes, they get sick and then their underlying disease gets worse and they come to the hospital and need to be hospitalized. … We are seeing a lot of exacerbation of underlying disease and we still see some pure COVID pneumonias, some of the classic COVID patients we saw through all the other surges in the pandemic.”
“The thing is you have to treat them the same,” Jansen said. “The requirements for PPE, the requirements for isolation. The labor-intensive care is no different whether the person came in and incidentally had COVID, meaning they came in with something else, or they came in with a condition exacerbated by COVID or COVID itself.”
“The stress on the staff is about the same.”
Q: And how is a seemingly milder variant leading to so many hospitalizations? Jansen explains.
A: “First of all, although omicron may not cause as severe an illness, particularly in respect to some of the COVID pneumonias, this is a math problem. If you have a variant that is four times more infectious and is only half as virulent or only causes half as severe disease, you are still increasing the number of people who come to the hospital.”
A measure of infectiousness is “R0″ pronounced “R-naught” and represents the number of new infections estimated to stem from a single case. In other words, if the R0 is two, then one person with the disease is expected to infect, on average, two others.
“It really is a matter of the number of people who are infected. Omicron is as infectious as anything we’ve ever seen. Some people compare it to as infectious as measles. It’s R-naught is probably 10 or 11 compared to the previous highest one we saw was probably six, so at least twice as infectious as other variants have ever been.”
“So the sheer numbers of people who are positive, a certain percentage of those are going to get sick and they are the ones who wind up in the hospital,” Jansen said. “We are seeing, we have record numbers of patients who are COVID-positive who are in the ICU. This is once again because of the sheer numbers of people who have come to the hospital. When you have this many people infected it is just as devastating from a society and therefore from a hospital perspective.
“We are seeing deaths, directly related to COVID.”

Q: What’s this latest wave like for health care workers? Dr. James E. Black, director of emergency services at Phoebe Putney Memorial Hospital in Albany shares his thoughts.
A: “It’s different. It’s shifted. Early on, everybody dove in with both feet taking care of everyone they could and we put the needs of patients and population above our own health, but as the pandemic became more prolonged we had to find a way to sustain that energy and that drive. And that hope and anticipation this would be a blip in historical significance, well, we kept having more surges and we realized this is more of a marathon than a sprint. Then you throw in things like the decisive nature of vaccination status and the changing nature of the disease and all of the variables, and all of the different challenges, we do our best to keep taking care of ourselves while also at the same time learning to function in a world where COVID is going to continue to exist. We have to try to make sure not to get too frustrated. We keep pressing ahead.”