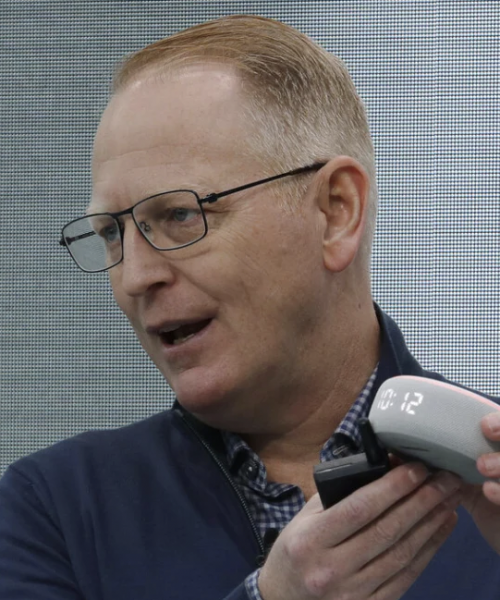
By Michael Ollove, Stateline.org
Troy Warren for CNT #Health
Remote health services soared during the pandemic, opening the eyes of many medical providers and patients
Before the COVID-19 pandemic, medical executive Lyndi Church and her colleagues at Caring Hands Healthcare Centers in southeastern Oklahoma had been intrigued by telehealth, but they feared it was unworkable in their rural corner of the state.
Many residents of the area lacked reliable broadband or didn’t have the devices or technological savvy to use telehealth services. Church, the chief operations officer of Caring Hands, anticipated significant resistance. “We weren’t sure how our patients would take to it,” she said.
Then the pandemic hit, and everything changed.
Early on, Caring Hands stopped treating patients in its facilities. Health workers saw some patients in the centers’ parking lots, but other than that, Church said, all medical care occurred virtually. To her surprise, despite occasionally spotty mobile and broadband service, patients took to telehealth.
“The majority of our patients were incredibly appreciative of the service, especially when they were so fearful about coming into an office,” she said.
The use of remote health services soared during the pandemic, opening the eyes of many medical providers and patients to telehealth’s convenience, efficiency and relative low cost. But its future depends largely on whether state lawmakers extend emergency measures that made telehealth a viable alternative for patients and providers wary of in-person contact. The most important changes most states made were to expand Medicaid coverage to different types of virtual appointments and to enact telehealth coverage requirements for private insurers.
Mei Wa Kwong, executive director of the Center for Connected Health Policy, a nonpartisan organization widely regarded as an authority on telehealth, estimates that the number of telehealth visits increased by as much as 40% during spring and summer 2020 and remains 30% higher than it was before the pandemic. According to a survey conducted by the National Association of Community Health Centers, the percentage of health centers using telehealth jumped from 43% before the pandemic to 98% during the early months of the crisis.
“The telehealth temporary policies helped so many people receive care they otherwise wouldn’t have received or may have put off getting until it became a more serious issue,” Kwong wrote in an email to Stateline. “To suddenly have that access taken away by a policy change could have significant, adverse impacts on many.”
Many states already have extended temporary telehealth measures that were set to expire with the lifting of public health emergencies, and other states are considering doing the same. Kwong estimates that there are more than 1,000 telehealth bills pending in state legislatures, many of which would allow more services to be provided virtually or mandate that public or private insurers cover them.
No organized opposition has emerged to the legislation, though it’s unclear how much providers will want to use telemedicine once their patients feel less anxious about exposure to the coronavirus.
“It is all about change management, teaching people to do things differently in their practices,” said Mary Zelazny, CEO of Finger Lakes Community Health in rural upstate New York, which used telehealth before the pandemic but ramped up during the crisis.
Telehealth, she said, has increased the efficiency of her health centers, saved money and improved care.
“We’re not going back.”
Many of the pending telehealth bills pertain to Medicaid, the joint federal/state health plan for low-income Americans. Twenty-seven states already have taken advantage of relaxed federal rules to expand Medicaid coverage of telehealth services, according to the National Conference of State Legislatures.
For example, many states, including Arkansas, Connecticut, Kentucky and Vermont, permanently authorized Medicaid coverage for audio-only medical consultations, without a video component. Colorado, Kentucky and Mississippi enacted legislation to ensure post-pandemic Medicaid reimbursement for telehealth services delivered by community health centers. And New Hampshire from now on will require its Medicaid program to pay providers the same amount for telehealth and in-person visits.
Arkansas also approved a law permanently extending Medicaid coverage to a raft of behavioral health and substance use services delivered through telehealth. The state’s Medicaid program now covers remote therapy provided by psychologists, clinical social workers, and marriage and family counselors. It also covers crisis intervention, substance use assessments, group therapy for those over 18 and mental health diagnosis assessments for patients under 21. Both chambers of the Arkansas legislature approved the measures last spring without a dissenting vote.
Dr. Lee Johnson, a Republican state representative who sponsored the Arkansas bill, said during the pandemic he came to appreciate that behavioral health services were particularly suited to telehealth. Generally, there is no need for a physical examination or lab work, and it gives greater privacy to patients who may be worried about the stigma of visiting a mental health provider.
“If you’re in a small community or even bigger communities and you have to go to psychologist or psychiatrist, maybe you’re nervous that someone will see you,” said Johnson, an emergency room physician. “This gives you the anonymity of being able to be at home and still accessing those services.”
Congress cleared the way for states by allowing Medicaid and Medicare to pay providers for telehealth services delivered to patients in their homes while also lifting the limited restrictions on where providers could be located. It also extended coverage to different types of telehealth services and providers and to audio-only appointments, which were previously excluded.
Taking advantage of the new rules, Colorado made telehealth services provided by physical therapists, occupational therapists, hospice care workers, home health providers and pediatric behavioral health specialists eligible for Medicaid reimbursement. The state also specified that home health agency services and therapies, hospice care and pediatric mental health services could be provided over the telephone. However, all the changes are tied to Colorado’s ongoing public health emergency, and it’s unclear whether they will be extended beyond that.
Medicare, the public health plan for older Americans, also loosened many of its telehealth reimbursement rules during the pandemic. The Biden administration announced this summer that Medicare will continue to cover virtual behavioral health services, but that the federal Centers for Medicare and Medicaid will evaluate other telehealth services before deciding whether to extend coverage beyond 2024.
Proponents of telehealth, including the National Association of Community Health Services, are pushing Congress to make the changes permanent.
More than two dozen states also have made permanent some telehealth coverage requirements for private insurers. For example, after the pandemic is over, Arizona, Iowa, Massachusetts and New Hampshire will require private insurers to cover all telehealth services and to reimburse providers at the same rate as in-person services. At least four states—Massachusetts, North Dakota, Vermont and Washington—extended the requirement for private insurers to reimburse for audio-only consultations, though not necessarily permanently.
The state laws on private insurers generally apply only to individual health insurance policies or those to which an employer does not contribute. Employer-funded plans are regulated by the federal government.
Although patients have embraced telehealth options during the pandemic, that is no guarantee that they will continue to do so once it is over. Kim Schwartz, CEO of the Roanoke Chowan Community Health Center in a rural area of eastern North Carolina, said that at the height of the pandemic, 90% of primary care visits were held virtually. Now, 80% of her patients come for in-person visits, even if it means long drives.
“Culturally, the dynamic of convenience wasn’t as high a value as the in-person relationship,” she said.
Schwartz noted that broadband availability and computer literacy remain barriers. Nevertheless, she said, telehealth must be part of her center’s future because of the advantages it offers in terms of stretching limited staff resources. The challenge, she said, is to increase the comfort level of her patients.
Rural areas aren’t the only ones with barriers to more use of telehealth. Dr. Sachin Shah, an internist and researcher at University of Chicago Medicine, studied the racial disparities in the use of telehealth on the South Side of Chicago during the pandemic. Many of his Black patients live in urban neighborhoods that, as in rural areas, struggle with broadband access, computer literacy and technology availability.
“That leaves a huge, really vulnerable segment of our patient population behind,” Shah said. Many of his older Black patients who do not own smartphones, he said, benefited from temporary changes that made telephone consultations reimbursable. Policymakers, he said, must consider inequities as they draft telehealth measures.
Despite the barriers and the unique circumstances of the pandemic that brought telehealth to the forefront, many in health care insist the service has proved its value in complementing in-person medical care.
“This wasn’t the result of great planning; it fell into our laps,” said Shah. “But it’s such a great opportunity. I would hate to see us go backward.”
In Other NEWS